Scientists have suggested using the flu vaccine as an additional anti-tumor therapy. They tested their method on mice and found that the vaccine stops tumorgrowth…. Precision medicine is currently emerging as a tool that seeks to make cancer treatment more effective, an issue that was highlighted during the 6th Annual… Multiple myeloma cancer life expectancy , Each form of cancer is characterized by an independent malignant growth of a specific cell type in the body…. Until some years ago, treat multiple myeloma had a life expectancy of 3 to 4 years, but now the quality and years of life of…Multiple myeloma and flu vaccine
Precision medicine, the future in cancer treatment
Multiple myeloma cancer life expectancy
Multiple myeloma stage 3 life expectancy
A Category
Multiple myeloma and flu vaccine
Scientists have suggested using the flu vaccine as an additional anti-tumor therapy. They tested their method on mice and found that the vaccine stops tumorgrowth. This works even in those mice that have been “infected” with human tumors, meaning it can theoretically work on us. The work was published in PNAS. One of the main…
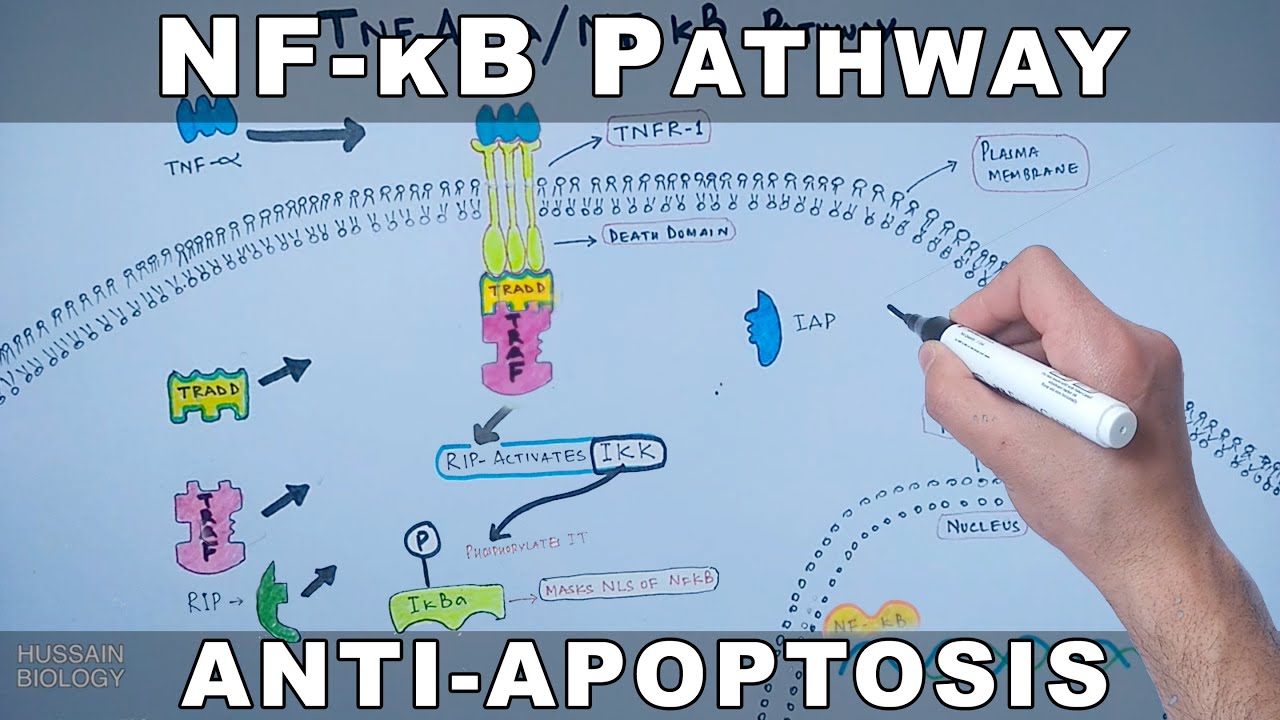
Precision medicine, the future in cancer treatment
Precision medicine is currently emerging as a tool that seeks to make cancer treatment more effective, an issue that was highlighted during the 6th Annual Meeting of the Mexican College for Cancer Research (C-MIC). Dr. Luis Alonso Herrera Montalvo, director of the National Institute of Genomic Medicine and founder of CMIC, explained that, although the…